Clinical Reasoning for Perplexing Clients
Clinical Reasoning for Perplexing Clients
Navigating Chronic Pain and the Biopsychosocial Model
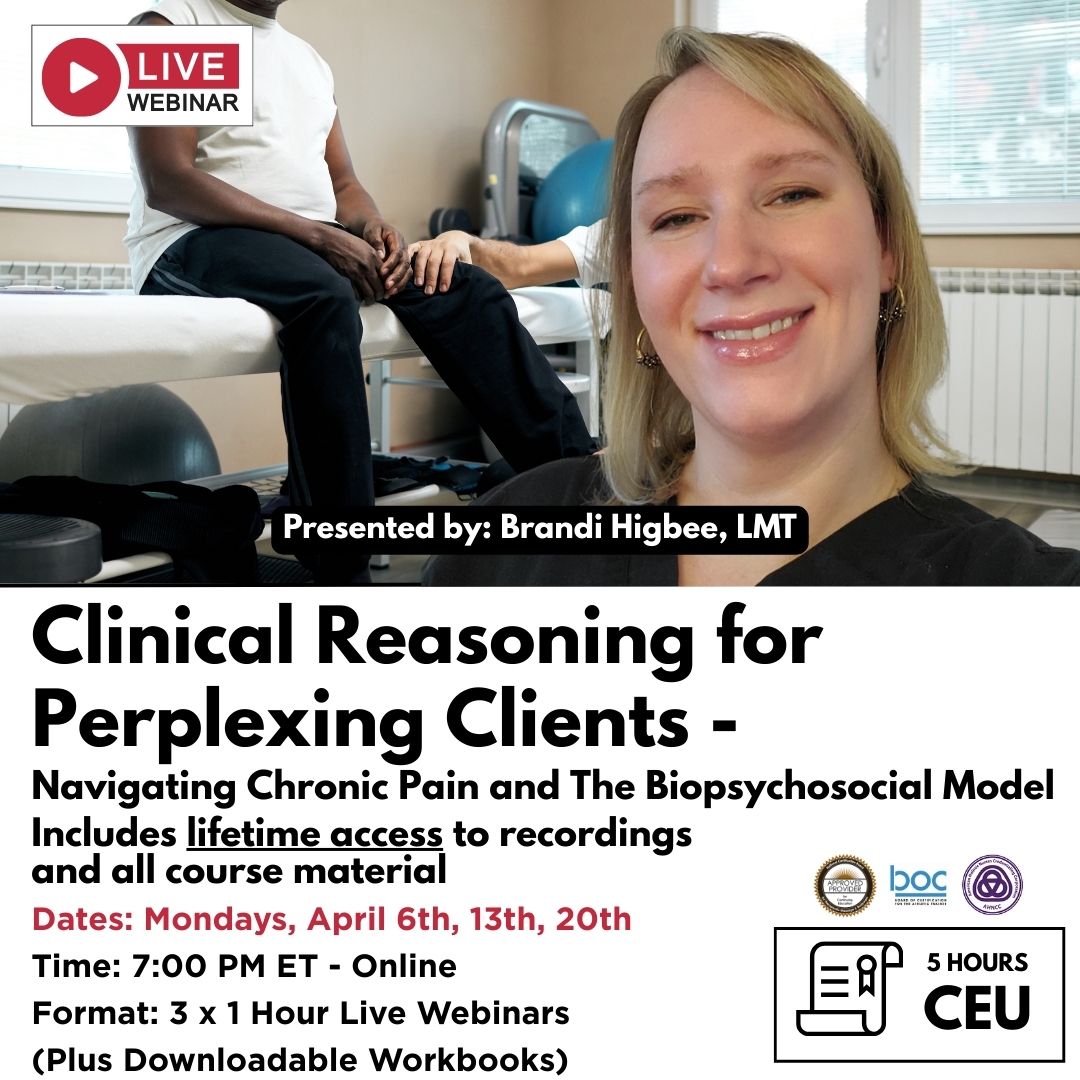
3-Part Live CE Webinar Series with Brandi Higbee
Mondays, April 6, 13, 20 • 7:00–8:00 PM ET
Live Online • 5 CE Hours • Includes Lifetime Access
Are you working with clients experiencing acute or chronic pain — especially those who say, “I don’t know what I did… the pain just started and won’t go away”?
Have you ever felt unsure how to proceed when standard assessment and treatment approaches don’t seem to fit?
This webinar series is designed for you.
Presented by Brandi Higbee, this 3-part live webinar explores how massage therapists and manual practitioners can develop clearer clinical reasoning when working with complex, persistent, or confusing pain presentations — using a biopsychosocial lens that stays firmly within scope of practice.
Course Overview
This series focuses on improving how therapists think, listen, assess, and plan — not just what techniques they use. Drawing from clinical experience and current pain-informed frameworks, Brandi guides participants through a structured yet flexible reasoning process that supports safer, more effective sessions for clients with chronic or perplexing pain.
You’ll learn how posture, abdominal tension, nervous system state, prior trauma, stress, and client expectations can all influence pain — often more than the specific technique applied.
Across three sessions, participants will explore:
How to build effective session plans beyond the standard SOAP format
Why some tissues remain tense despite repeated treatment
How pressure, communication, and pacing influence nervous system safety
The role of abdominal anatomy in pain experienced elsewhere in the body
How to apply the biopsychosocial model ethically within massage therapy
When pain is modifiable — and when it is not your responsibility to “fix”
Learning Objectives
By the end of this webinar series, participants will be able to:
Identify five essential clinical reasoning questions that guide effective session planning
Recognize the body’s motivations for maintaining muscular and fascial tension
Evaluate how therapeutic pressure communicates safety to the nervous system
Review abdominal anatomy and its role in widespread chronic pain patterns
Analyze postural dynamics related to persistent pain presentations
Apply the biopsychosocial model within the scope of massage therapy
Improve client education before, during, and after sessions
Develop stronger active listening skills to support treatment decisions
Identify contributing factors behind common presentations such as piriformis syndrome, non-specific low back pain, chronic hip, shoulder, and neck pain
Demonstrate professional draping and communication practices
Webinar Schedule & Content
Session 1 — April 27
Lecture: Clinical Reasoning & the Biopsychosocial Model
An in-depth exploration of the mental, emotional, and physical factors clients bring into the treatment room — and how these influence outcomes.
Topics include:
Client lived experience and its impact on pain
Stress levels, trauma history, fears, beliefs, outlook, and support systems
Common pain complaints and their relationship to abdominal tension and posture
Bio-tensegrity and force transfer principles
Upper and lower cross syndromes
Five Key Clinical Questions:
-
What is their posture telling us?
-
What are their goals for today’s session?
-
Are there prior injuries, surgeries, or accidents?
-
What state is their nervous system in?
-
What is not my responsibility? — staying in scope and knowing when massage is palliative versus alleviating
Includes discussion on client education, managing expectations, and treatment planning for single vs. multiple sessions.
Session 2 — May 4
Live Hands-On Treatment Demonstration with Model
A practical, treatment-room–based session focusing on abdominal work, lower body integration, and posterior chain assessment.
Content includes:
Supine abdominal techniques with safe, professional draping
Anatomical review using a physical model
Rectus abdominis, obliques, aponeuroses, diaphragm, psoas, and iliacus
Lines of force transfer from hips to shoulders through the abdomen
Key palpation landmarks
Discussion of trauma-related tension and stress response
Lower body integration:
Supine adductors and IT band dynamics
Relationship to low back, hip, and SI joint pain
Prone work:
Differentiating piriformis syndrome from other pain drivers
Glute strength, compensation patterns, and assessment
Lumbodorsal fascia and non-specific low back pain
Time permitting: ischial tuberosity and posterior chain integration.
Session 3 — May 11
Live Q&A with Brandi Higbee
An open, interactive session dedicated to participant questions, case discussions, and deeper clarification of concepts from Days One and Two.
Who This Course Is For
This webinar series is ideal for:
Massage Therapists
Manual and Bodywork Practitioners
Rehabilitation-focused Therapists
Clinicians working with chronic or complex pain presentations
No advanced pain science background is required — just a desire to improve clinical reasoning and client outcomes.
What’s Included
Three live, instructor-led webinars (1 hour each)
Lifetime access to all session recordings
Fully illustrated downloadable workbook
Continuing education exam
Certificate of completion
All recordings and materials remain accessible indefinitely, allowing you to revisit the content at your convenience.
Join Brandi Higbee for this thoughtful, practical exploration of chronic pain, clinical reasoning, and the biopsychosocial model — and gain tools to work more confidently with your most perplexing clients.

NAT Certificates are issued for all courses and can be downloaded and printed online at no additional charge. Presentation frame not included.