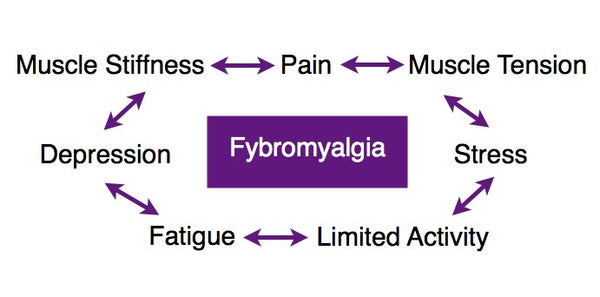
Trigger Point Therapy - Fibromyalgia
Fibromyalgia - Why Your Diet May Be an Important Factor in Managing the Pain
More women than men are affected by fibromyalgia, but there is no age profile, and currently no reliable research to account for the gender factor
Because the cause of this "obviously very real" disorder remains unknown, too many patients are left disappointed by medical doctors who offer little in the way of hope or relief.
Patients who present in our clinics with fibromyalgia are undoubtedly amongst the most highly motivated to seek treatment and relief.
We don't yet have the answers to treating this condition but we do know that we can often provide effective relief, even if only short term, with the use of a number of manual therapy techniques, almost always involving the treatment of trigger points.
“Fibromyalgia is a complex syndrome characterized by pain amplification, musculo-skeletal discomfort, and systemic symptoms” (Starlanyl & Copeland 2001).
Fibromyalgia means pain in the fibrous, connective, and tendinous tissues of the body, and fibromyalgia syndrome is characterized by widespread diffuse musculoskeletal pain and fatigue.
Fibromyalgia and Trigger Points
Like myofascial trigger points, fibromyalgic pain arises from the connective tissues, muscles, tendons, and ligaments; similarly, fibromyalgia does not involve the joints. Myofascial trigger points and fibromyalgia are often mistaken for each other; however, they are discrete conditions.
Unlike trigger point manifestation, fibromyalgia is believed to have a systemic (CNS) origin. Starlanyl & Sharkey (2013) reviewed the current evidence and assert that, while fibromyalgia and MTPs are distinct entities, both are maintained by central and/or peripheral sensitization (see below).
Whilst trigger points cause a specific and reproducible pattern of pain referral, patients with fibromyalgia describe that they “ache all over” (although some do describe localized tender spots). Patients with fibromyalgia also describe their muscles as feeling like they have been “pulled” or overworked. Sometimes the muscles twitch and at other times they burn.
Peripheral and Central Sensitization
Pain is a complex area of medicine, and current research has thrown up a number of discoveries relevant to trigger point manifestation and perpetuation. Pain systems need to be sensitive enough to detect potentially harmful stimuli.
But in the case of trigger points, these systems eventually become too sensitive, causing us pain with no benefit.
Hypersensitivity arises because our pain pathways actually increase in sensitivity when they relay pain messages, and, with regard to MTPs, the mechanisms of this sensitization are now coming to light.
Peripheral Sensitization
Within 48 hours of developing, and if untreated, MTPs cause inflammation, chronic facilitation, and changes in feedback from the host muscle.
Physiologically, there is a drop in the excitation threshold of polymodal nociceptors so that even normally innocuous, light stimuli activate them.
After sensitization of “pain fibers,” stimuli that as a rule are non-painful can cause pain (Schaible 2006); in addition, mechano-insensitive nerve fibers can become mechano-sensitive.
“This recruitment of silent nociceptors adds significantly to the nociceptive input to the spinal cord. Resting discharges may be induced or increased in nociceptors” (Schaible 2006).
This occurs because of chronic active trigger points providing a continuous afferent barrage into the spinal cord.
The suspected mechanism is:
-
Substance P, released from nociceptor terminals, carries nociceptive signals
for central processing, and alters local microcirculation and vessel permeability, leading to local edema, activating both mechanoreceptors and nociceptors, with subsequent increased tenderness and pain. -
Persistent activation with these algogenic substances leads to changes in nociceptor responsiveness both peripherally and centrally.
It has been shown that up to 50% of muscle nerves may be made up of nociceptors, and that nociceptors also innervate the connective tissue surrounding muscle. This could account for the severity of pain and exquisite tenderness found in muscles on palpation. Persistent activation of nociceptors leads to peripheral sensitization whereby primary afferent nociceptors exhibit an enhanced responsiveness to natural stimuli.
Central Sensitization (Spinal Hyperexcitability)
In the course of time the peripheral changes move deeper into the nervous system and the pattern becomes established centrally.
The superficial, the deep, and the ventral spinal cord show pronounced changes in their response properties (Schaible 2006).
This is a form of neuroplasticity: after sensitization, an increased percentage of neurons in a segment respond to stimulation of an inflamed tissue.
The sensitivity of the spinal cord neurons becomes enhanced, so that an input that was previously subthreshold may now be sufficient to activate the neurons.
This effect is magnified up and down the spinal cord over several segmental levels both caudally and cephalically, which may lead to lowered activation thresholds for other MTPs.
The implications of this are profound: it may well be that a chronic trigger point in one area may sensitize levels of the spinal cord above and below the input level.
Over time, this may lead to a type of neuroplastic change in the CNS. This will decrease the pain threshold in other regions remote from the original source and possibly lower the threshold potential for other trigger points within the pain map.
Central sensitization can persist for weeks, months, and even years, depending on the chronicity of the stimulus.
The suspected mechanism is:
-
Continuous activation of muscle nociceptors— induces neuroplastic changes and sensitization of dorsal horn neurons.
-
Nociceptive input from skeletal muscle—far more effective at inducing neuroplastic change in the spinal cord than noxious input from the skin.
- Repetitive stimulation of primary afferent nociceptors leading to a progressive increase in action potential discharge—a phenomenon called windup, which may lead to a 20-fold increase in neuronal sensitivity.
-
The result is an increase in intensity of pain and sensitization of neurones in the dorsal horn of the spinal cord because of the activation of N-methyl-D-aspartate (NMDA) receptors— central sensitization.
-
Sensory neurones from the dorsal root ganglia become sensitized to mechanical stimuli, so that only mildly painful stimuli become more painful—mechanical hyperalgesia.
-
Sustained nociceptive input from active trigger points may not only sensitize dorsal horn neurons, leading to hyperalgesia and allodynia, but also generate expanded referred pain regions.
Potential mechanisms for this phenomenon are the activation of previously redundant synapses at the dorsal horn, and the sprouting of new spinal terminals that broaden synaptic contacts at the dorsal horn, which may explain the referred pain seen with active trigger points.
Both peripheral and central sensitization can have serious unwanted effects: the advice therefore is to interfere with this process as soon as possible.
The good news is that myofascial trigger point release and dry needling techniques have both been reliably demonstrated to reduce these effects.
Find a Trigger Point Professional in your area
More Articles About Fibromyalgia
Dry Needling for Trigger Points
Certify as a Trigger Point Therapist
NAT Online Courses:
This trigger point therapy blog is intended to be used for information purposes only and is not intended to be used for medical diagnosis or treatment or to substitute for a medical diagnosis and/or treatment rendered or prescribed by a physician or competent healthcare professional. This information is designed as educational material, but should not be taken as a recommendation for treatment of any particular person or patient. Always consult your physician if you think you need treatment or if you feel unwell.
About Niel Asher Education
Niel Asher Education (NAT Global Campus) is a globally recognised provider of high-quality professional learning for hands-on health and movement practitioners. Through an extensive catalogue of expert-led online courses, NAT delivers continuing education for massage therapists, supporting both newly qualified and highly experienced professionals with practical, clinically relevant training designed for real-world practice.
Beyond massage therapy, Niel Asher Education offers comprehensive continuing education for physical therapists, continuing education for athletic trainers, continuing education for chiropractors, and continuing education for rehabilitation professionals working across a wide range of clinical, sports, and wellness environments. Courses span manual therapy, movement, rehabilitation, pain management, integrative therapies, and practitioner self-care, with content presented by respected educators and clinicians from around the world.
Known for its high production values and practitioner-focused approach, Niel Asher Education emphasises clarity, practical application, and professional integrity. Its online learning model allows practitioners to study at their own pace while earning recognised certificates and maintaining ongoing professional development requirements, making continuing education accessible regardless of location or schedule.
Through partnerships with leading educational platforms and organisations worldwide, Niel Asher Education continues to expand access to trusted, high-quality continuing education for massage therapists, continuing education for physical therapists, continuing education for athletic trainers, continuing education for chiropractors, and continuing education for rehabilitation professionals, supporting lifelong learning and professional excellence across the global therapy community.

Continuing Professional Education
Looking for Massage Therapy CEUs, PT and ATC continuing education, chiropractic CE, or advanced manual therapy training? Explore our evidence-based online courses designed for hands-on professionals.