Plantar Fasciitis Relief: Expert Advice and Self-Help Strategies
Plantar Fasciitis: Understanding, Treating, and Overcoming Heel Pain
Plantar fasciitis. The name itself sounds a bit intimidating, and the pain it causes can certainly be just that. If you've ever experienced a sharp, stabbing pain in your heel, especially first thing in the morning or after a period of rest, you might be familiar with this common culprit of foot pain. This article delves into the intricacies of plantar fasciitis, exploring its causes, symptoms, diagnosis, and a comprehensive range of treatment options, including a look at how acupuncture, massage, trigger point therapy, cupping, and taping can offer relief.
What is Plantar Fasciitis?
Plantar fasciitis is an inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of your foot, connecting your heel1 bone (calcaneus) to your toes. Think2 of it as a strong, supportive arch for your foot. The plantar fascia plays a crucial role in supporting the arch of your foot, absorbing shock, and helping you push off during walking and running.
When this vital tissue becomes overstretched or overused, it can develop tiny tears and inflammation, leading to the characteristic pain of plantar fasciitis. This pain is often most intense with the first few steps after waking up or after a period of inactivity, as the fascia tightens overnight or during rest. As you move around, the pain may lessen slightly, but it often returns or worsens with prolonged activity.
What Causes Plantar Fasciitis?
While the exact cause isn't always clear, several factors can contribute to the development of plantar fasciitis. These include overuse from activities like running or jumping, improper footwear lacking adequate arch support or cushioning, tight calf muscles restricting ankle flexibility, excess weight placing additional pressure on the feet, age-related loss of fascia elasticity, specific foot structures like flat feet or high arches, and a sudden increase in activity levels. Essentially, anything that overloads or strains the plantar fascia can lead to inflammation and pain.

Symptoms of Plantar Fasciitis
The hallmark symptom of plantar fasciitis is pain in the heel, typically felt on the underside of the foot. This pain is often described as sharp, stabbing, or aching, and is most intense in the morning or after rest. It may lessen with activity but often returns or worsens with prolonged use, and can be tender to the touch. Some people may also experience stiffness in the heel and arch.
Diagnosing Plantar Fasciitis
Diagnosis is usually based on a physical examination and a description of your symptoms. Your doctor or physical therapist will likely ask about your medical history and activity levels, palpate the plantar fascia, assess your foot and ankle range of motion, and observe your gait. In some cases, imaging tests like X-rays or MRIs may be used to rule out other conditions.
Treating Plantar Fasciitis: A Multifaceted Approach
The good news is that plantar fasciitis usually responds well to conservative treatment. A combination of the following therapies is often most effective:
Conservative Care: This is the cornerstone of plantar fasciitis treatment and often involves several approaches used in conjunction. Resting the foot and reducing aggravating activities is paramount. Ice application for 15-20 minutes several times a day can reduce pain and inflammation. Stretching the plantar fascia and calf muscles is crucial for improving flexibility and reducing tension. Supportive footwear with good arch support and cushioning is essential, and orthotics (custom or over-the-counter) can provide additional support. Night splints can help prevent the fascia from tightening overnight. Physical therapy can provide a tailored program of exercises, manual therapy, and modalities like ultrasound. Over-the-counter pain relievers like NSAIDs can help manage pain, but stronger medications should be used sparingly and only under medical supervision.
Massage Therapy: Massage can be a highly effective tool for plantar fasciitis. It helps to release tension in the plantar fascia itself, as well as in the surrounding muscles of the foot, ankle, and calf. Massage can improve blood flow to the area, promoting healing and reducing pain. Specific techniques like myofascial release can address restrictions in the fascia.
Trigger Point Therapy: Trigger points in the calf muscles, and sometimes even in the foot itself, can contribute to plantar fasciitis pain. Trigger point therapy involves applying sustained pressure to these specific points to release tension and alleviate referred pain. Addressing trigger points can be a key component of a comprehensive treatment plan.
Cupping Therapy: Cupping therapy, an ancient practice, can be beneficial for plantar fasciitis by increasing blood flow to the affected area and releasing muscle tension. The suction created by the cups helps to lift the tissue, promoting circulation and reducing inflammation.
Taping: Kinesiology taping can provide support to the arch of the foot, reducing strain on the plantar fascia. Taping can also help to improve proprioception (awareness of foot position) and can be used to offload pressure from painful areas.
Advanced Treatments: Acupuncture, extracorporeal shock wave therapy (ESWT), and, in rare cases, surgery.
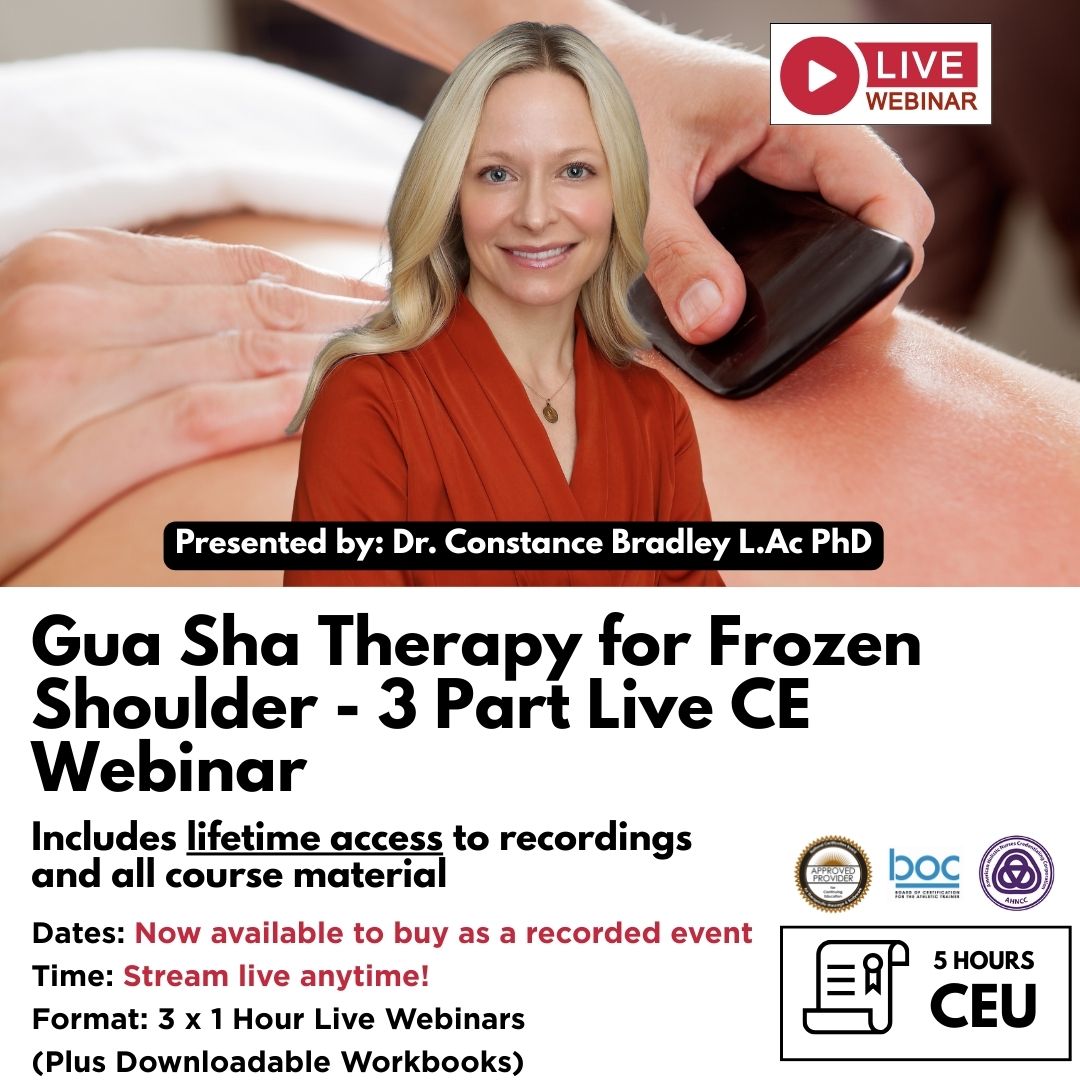
Acupuncture for Plantar Fasciitis
Acupuncture, a key component of Traditional Chinese Medicine (TCM), offers a unique approach to treating plantar fasciitis. TCM views pain as a disruption of energy flow (Qi) within the body. Acupuncture aims to restore this flow by inserting thin needles into specific acupoints along meridians. It may help by reducing inflammation, improving blood flow, relaxing muscles, and modulating pain signals. The accompanying video demonstrates a typical acupuncture treatment for plantar fasciitis. [Insert video here] Consult with a licensed acupuncturist experienced in treating musculoskeletal conditions.
Preventing Plantar Fasciitis
Preventing plantar fasciitis is often easier than treating it. Tips include wearing supportive shoes, stretching regularly, maintaining a healthy weight, gradually increasing activity levels, strengthening your core, replacing running shoes regularly, and considering custom orthotics.
When to See a Doctor
It's important to see a doctor if your pain is severe and does not improve with home care, if you experience numbness or tingling in your foot, or if you have any other concerns. Early intervention can help prevent plantar fasciitis from becoming a chronic problem.
About Niel Asher Education
Niel Asher Education (NAT Global Campus) is a globally recognised provider of high-quality professional learning for hands-on health and movement practitioners. Through an extensive catalogue of expert-led online courses, NAT delivers continuing education for massage therapists, supporting both newly qualified and highly experienced professionals with practical, clinically relevant training designed for real-world practice.
Beyond massage therapy, Niel Asher Education offers comprehensive continuing education for physical therapists, continuing education for athletic trainers, continuing education for chiropractors, and continuing education for rehabilitation professionals working across a wide range of clinical, sports, and wellness environments. Courses span manual therapy, movement, rehabilitation, pain management, integrative therapies, and practitioner self-care, with content presented by respected educators and clinicians from around the world.
Known for its high production values and practitioner-focused approach, Niel Asher Education emphasises clarity, practical application, and professional integrity. Its online learning model allows practitioners to study at their own pace while earning recognised certificates and maintaining ongoing professional development requirements, making continuing education accessible regardless of location or schedule.
Through partnerships with leading educational platforms and organisations worldwide, Niel Asher Education continues to expand access to trusted, high-quality continuing education for massage therapists, continuing education for physical therapists, continuing education for athletic trainers, continuing education for chiropractors, and continuing education for rehabilitation professionals, supporting lifelong learning and professional excellence across the global therapy community.

Continuing Professional Education
Looking for Massage Therapy CEUs, PT and ATC continuing education, chiropractic CE, or advanced manual therapy training? Explore our evidence-based online courses designed for hands-on professionals.