10 Trigger Points Associated with Lower Back Pain
10 Trigger Points Associated with Lower Back Pain – What Every Therapist (and Sufferer) Should Know
Lower back pain is one of the most common complaints among adults, affecting people from all walks of life. Whether it’s a weekend warrior who pushed too hard at the gym, a desk worker slumped over a laptop for hours, or a manual laborer dealing with years of wear and tear, the lower back is a frequent source of discomfort. But what many don’t realize is that the true source of their pain may not be in the lower back at all.
Trigger points—those pesky, hyper-irritable nodules found within tight bands of muscle—are often to blame. While they can form anywhere in the body, certain trigger points refer pain directly to the lower back, even when the actual problem lies elsewhere. For massage therapists, manual therapists, and even those struggling with chronic lower back pain themselves, understanding which muscles contribute to lower back pain and how to release them can make a world of difference.
Let’s dive into ten of the most common trigger points associated with lower back pain and explore how they can be identified, treated, and—most importantly—prevented.
1. Quadratus Lumborum – The Silent Culprit
The quadratus lumborum (QL) is often called the "joker of low back pain" because it mimics so many other issues. Located on either side of the lumbar spine, the QL connects the ribs to the pelvis and plays a key role in stabilizing the spine, especially during movements like bending and twisting.
When trigger points form in the QL, they often refer deep, aching pain into the lower back and hips, sometimes making it difficult to stand up straight. Many people with QL trigger points describe a feeling of being "locked up" or "crooked," with one side of the lower back pulling tighter than the other.
Pain from the QL can be mistaken for a herniated disc or even kidney pain, which is why it’s important for therapists to assess the muscle directly. Hands-on release techniques, combined with gentle stretching and heat therapy, can provide significant relief.
2. Gluteus Medius – The Hidden Source of "Sciatica"
Many people who complain of lower back pain also experience radiating discomfort down the leg. While this is often labeled as sciatica, the true cause may be trigger points in the gluteus medius muscle.
Located on the side of the hip, the gluteus medius plays a key role in pelvic stability. When it develops trigger points, it can refer pain into the sacroiliac joint, lower back, and even down the outer leg—closely mimicking sciatic nerve pain. Unlike true sciatica, which is caused by nerve compression, gluteus medius trigger points respond well to manual therapy, stretching, and strengthening exercises.
3. Gluteus Maximus – More Than Just a Powerful Muscle
The gluteus maximus, the largest muscle in the body, is often associated with power and strength, but when trigger points develop within it, they can send aching pain into the sacrum and lower back.
Tightness in the glutes can be linked to prolonged sitting, poor posture, or inadequate hip mobility. Releasing these trigger points through deep tissue massage, foam rolling, and movement-based therapies can help restore proper function and reduce compensatory strain on the lower back.
4. Piriformis – The "Pain in the Butt" Muscle
The piriformis is a small, deep muscle that runs beneath the gluteus maximus, connecting the sacrum to the femur. While it plays a crucial role in hip rotation, when it develops trigger points, it can become a major contributor to lower back pain.
Many people are familiar with piriformis syndrome, where the muscle tightens and compresses the sciatic nerve. But even without true sciatic nerve involvement, piriformis trigger points can mimic sciatica, referring pain into the lower back, buttocks, and down the leg.
Stretching, myofascial release, and targeted massage can help keep the piriformis functioning properly and prevent unnecessary strain on the lower back.
5. Iliopsoas – The Overlooked Core Muscle
When people talk about "core strength," they often think of the abdominal muscles, but the iliopsoas (a combination of the iliacus and psoas major) is just as important. This deep hip flexor connects the lower spine to the thigh bone and plays a critical role in stabilizing the lumbar spine.
Trigger points in the iliopsoas can cause deep, aching pain in the lower back, groin, and front of the thigh. Since the iliopsoas is often tightened by prolonged sitting, many people with lower back pain have underlying dysfunction in this muscle.
Because of its depth, treating the iliopsoas requires specific manual therapy techniques, such as psoas release work and guided breathing exercises.
6. Rectus Abdominis – The Surprising Link Between the Core and the Back
Most people associate the rectus abdominis (the "six-pack" muscle) with aesthetics, but when trigger points develop within it, they can refer pain directly into the lower back.
Chronic tension in the abdominals—often caused by poor posture, overuse, or even emotional stress—can lead to tight bands of tissue that pull on the lower spine, creating discomfort. Addressing these trigger points, along with encouraging proper core activation, can help restore balance between the front and back of the body.
7. Erector Spinae – The Workhorses of the Spine
The erector spinae are a group of long, rope-like muscles that run along the length of the spine, helping to keep us upright. When these muscles develop trigger points, they can create a deep, burning pain in the lower back, often worsening with prolonged standing or bending.
Since the erector spinae are constantly engaged, they benefit from gentle stretching, mobility exercises, and deep tissue massage to prevent excessive tension buildup.
8. Latissimus Dorsi – The Upper Back Muscle That Affects the Lower Back
The latissimus dorsi, or "lats," is one of the largest muscles in the body, spanning from the upper back to the lower spine. While it’s often associated with shoulder movement, tightness in the lats can cause lower back pain, especially when lifting or reaching overhead.
Manual therapy targeting the lats, combined with mobility work for the thoracic spine, can help reduce compensation patterns that strain the lower back.
9. Hamstrings – The Back Chain Connection
Tight hamstrings pull on the pelvis, leading to postural imbalances that stress the lower back. Many people with chronic lower back pain have shortened hamstrings, contributing to anterior or posterior pelvic tilt.
Addressing hamstring trigger points through manual therapy, stretching, and dynamic movement exercises can relieve this tension and restore healthy pelvic alignment.
10. Tensor Fasciae Latae (TFL) – The Unsuspecting Instigator
The Tensor Fasciae Latae is a small but mighty muscle located at the front of the hip, playing a key role in stabilizing the pelvis and assisting in hip movement. When it becomes tight, it can refer pain into the lower back and sacral region, sometimes creating a deep ache that worsens with prolonged standing or walking.
Releasing TFL trigger points can be particularly helpful for athletes, runners, and individuals with hip dysfunction.
Bringing It All Together
Trigger points can be deceptive. Pain in the lower back doesn’t always originate in the lower back itself, and true relief often requires looking at the body as a whole. Understanding and addressing these key trigger points can transform how we approach lower back pain, whether as a therapist working with clients or as someone looking for long-term relief.
If you or your clients are dealing with persistent lower back pain, consider exploring these overlooked muscular sources—the solution may be just a trigger point away.
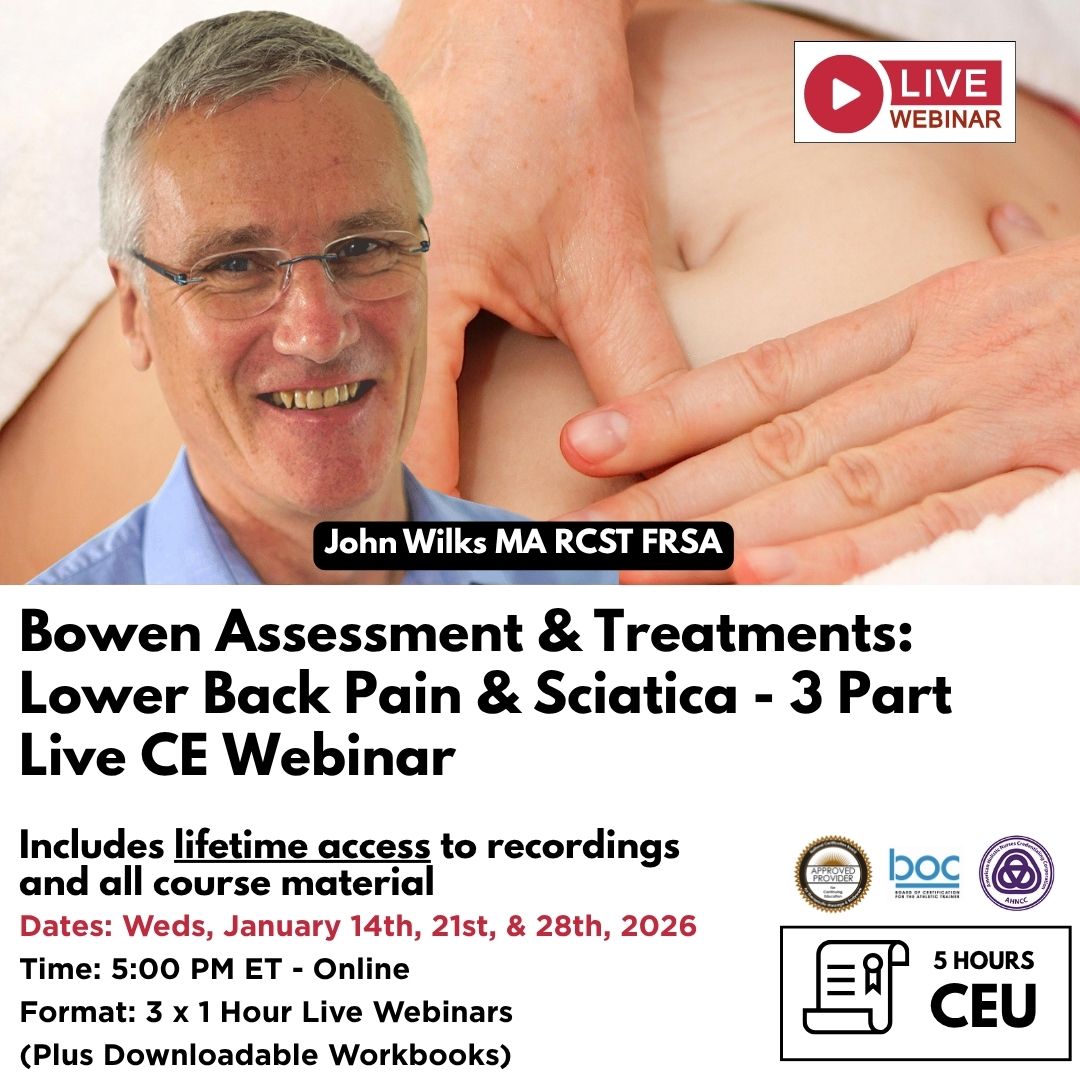
Further Your Knowledge in Trigger Point Therapy
For massage and manual therapists, understanding trigger points and their role in musculoskeletal pain is essential for providing effective treatment. Lower back pain is one of the most common complaints seen in clinical practice, and as we’ve explored, trigger points in multiple muscle groups can contribute to this condition. Developing the skills to accurately identify, assess, and treat these trigger points can transform your approach to client care, leading to better outcomes and long-term relief for those suffering from chronic pain.
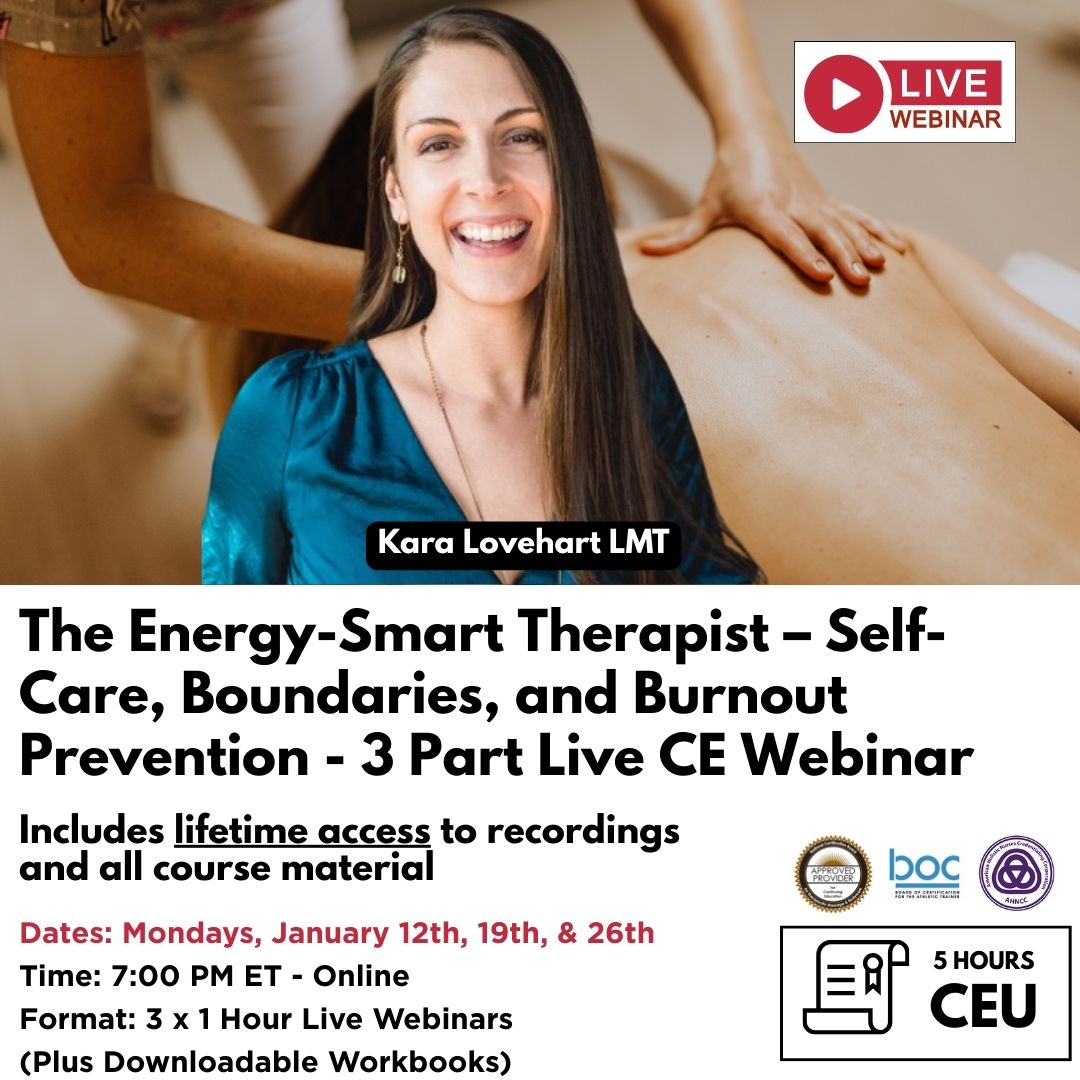
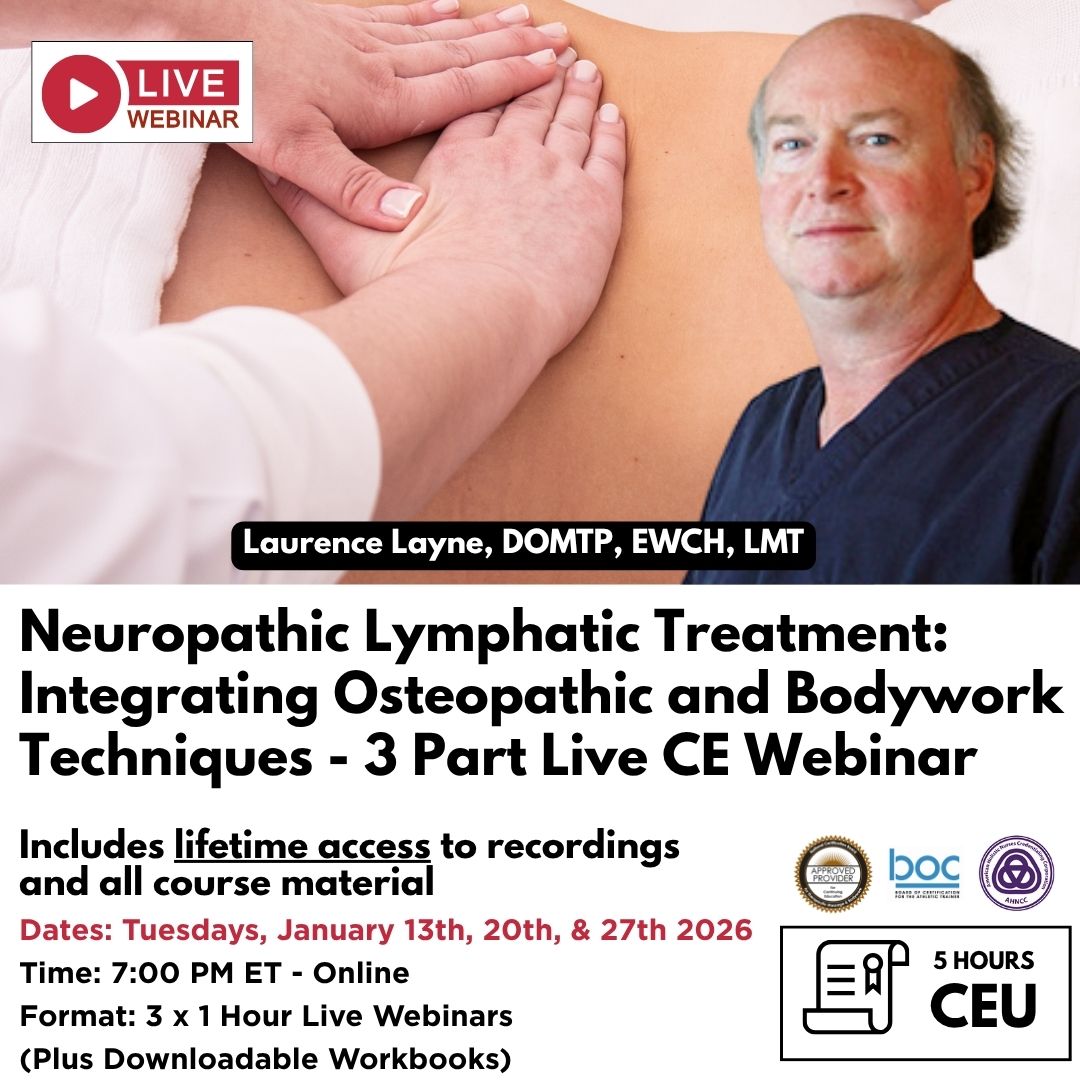
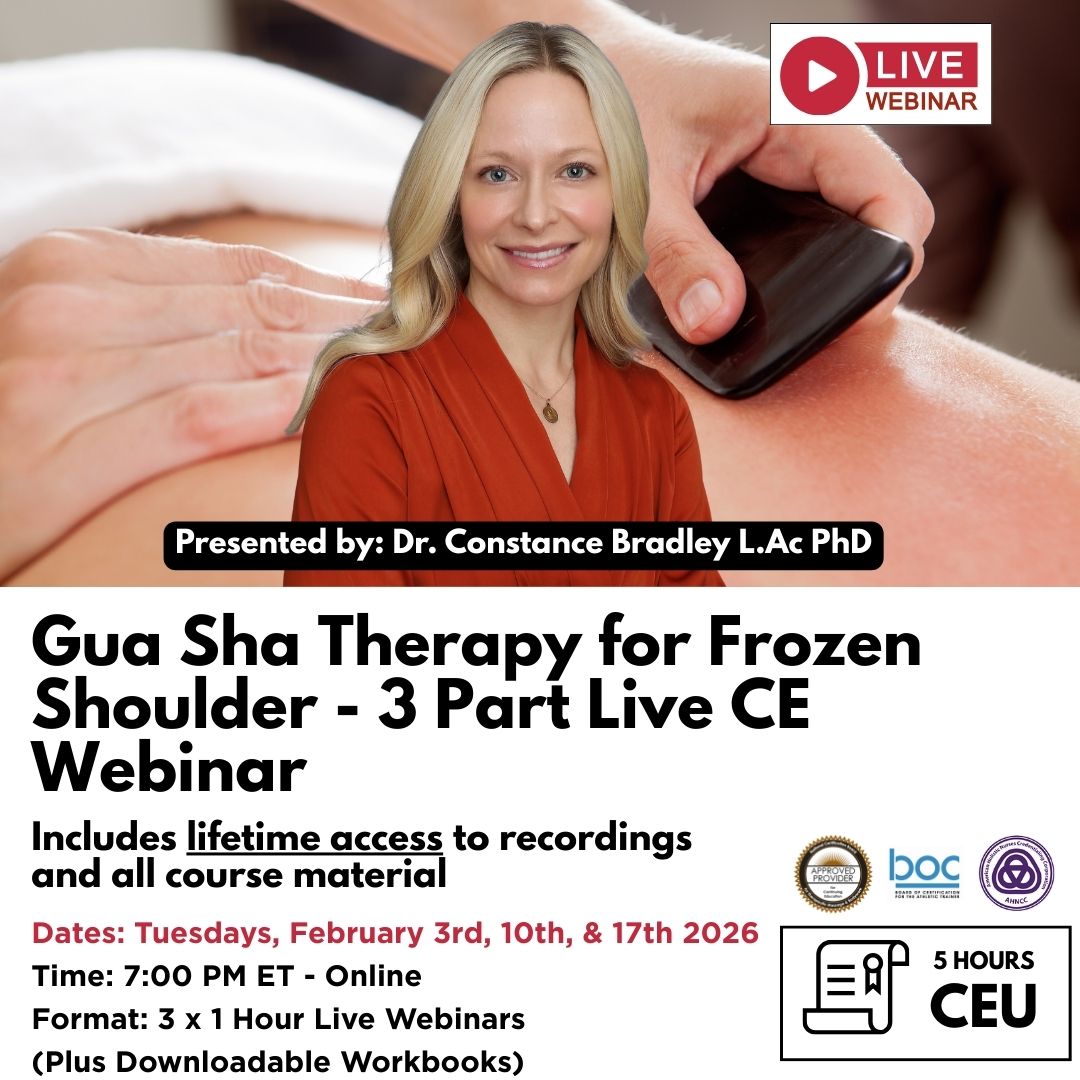
At Niel Asher Education (NAT), we offer a range of continuing education (CE), certificate, and diploma courses in trigger point therapy, myofascial release, and advanced manual therapy techniques. Our studio-filmed, evidence-informed courses are designed for therapists looking to enhance their skills, expand their practice, and stay ahead in the field of pain management and rehabilitation.
Explore Our Online Trigger Point Therapy Courses
If you’re looking to deepen your understanding of trigger points, myofascial dysfunction, and clinical applications, browse our online courses here. Whether you’re a massage therapist, manual therapist, physical therapist, chiropractor, or rehabilitation specialist, our courses provide:
- Accredited Continuing Education (CE) Hours recognized in multiple regions
- Comprehensive training in trigger point assessment and treatment techniques
- Specialist certifications and diploma programs to advance your professional development
- A flexible, self-paced online learning experience designed to fit your schedule
Thousands of therapists worldwide have trained with NAT to enhance their skills, grow their practice, and deliver outstanding results for their clients. Join our community of professionals dedicated to excellence in manual therapy and pain relief.
For more details on trigger point therapy training, click here.
References
- Travell, J. G., & Simons, D. G. (1999). Myofascial Pain and Dysfunction: The Trigger Point Manual, Volume 1: Upper Half of Body. Lippincott Williams & Wilkins.
- Travell, J. G., & Simons, D. G. (1992). Myofascial Pain and Dysfunction: The Trigger Point Manual, Volume 2: Lower Half of Body. Lippincott Williams & Wilkins.
- Fernández-de-Las-Peñas, C., Dommerholt, J. (2018). Trigger Point Dry Needling: An Evidence and Clinical-Based Approach. Elsevier Health Sciences.
- Simons, D. G. (2002). "Clinical and etiological update of myofascial pain from trigger points." Journal of Musculoskeletal Pain, 10(1), 115-121.
- Gerwin, R. D., Dommerholt, J., & Shah, J. P. (2004). "An expansion of Simons' integrated hypothesis of trigger point formation." Current Pain and Headache Reports, 8(6), 468-475.
Disclaimer
This article is for informational and educational purposes only and is not intended to replace professional medical advice, diagnosis, or treatment. If you are experiencing chronic or severe pain, consult a qualified healthcare provider before beginning any treatment. Manual therapy techniques should only be performed by trained professionals within their scope of practice.
About Niel Asher Education
Niel Asher Education (NAT Global Campus) is a globally recognised provider of high-quality professional learning for hands-on health and movement practitioners. Through an extensive catalogue of expert-led online courses, NAT delivers continuing education for massage therapists, supporting both newly qualified and highly experienced professionals with practical, clinically relevant training designed for real-world practice.
Beyond massage therapy, Niel Asher Education offers comprehensive continuing education for physical therapists, continuing education for athletic trainers, continuing education for chiropractors, and continuing education for rehabilitation professionals working across a wide range of clinical, sports, and wellness environments. Courses span manual therapy, movement, rehabilitation, pain management, integrative therapies, and practitioner self-care, with content presented by respected educators and clinicians from around the world.
Known for its high production values and practitioner-focused approach, Niel Asher Education emphasises clarity, practical application, and professional integrity. Its online learning model allows practitioners to study at their own pace while earning recognised certificates and maintaining ongoing professional development requirements, making continuing education accessible regardless of location or schedule.
Through partnerships with leading educational platforms and organisations worldwide, Niel Asher Education continues to expand access to trusted, high-quality continuing education for massage therapists, continuing education for physical therapists, continuing education for athletic trainers, continuing education for chiropractors, and continuing education for rehabilitation professionals, supporting lifelong learning and professional excellence across the global therapy community.

Continuing Professional Education
Looking for Massage Therapy CEUs, PT and ATC continuing education, chiropractic CE, or advanced manual therapy training? Explore our evidence-based online courses designed for hands-on professionals.