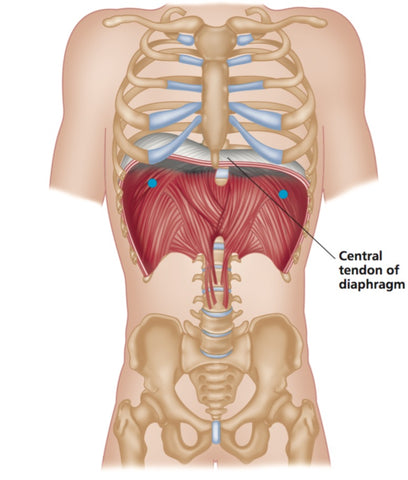
The Diaphragm and Breathing - Trigger Point Therapy
How To Assess and Influence Your Breathing
Abnormal breathing mechanics may be one of the key factors in the development of chronic myofascial trigger points throughout the body
Trigger point therapy can be a useful tool in releasing the musculoskeletal component of respiratory dysfunction and is especially useful when combined with other modalities, such as yoga, Feldenkrais, meditation, the Buteyko method and “breath therapy.”
Nothing in the body happens in isolation, and an exploration of breathing mechanics exemplifies this.

Breathing involves many sequences of coordinated muscular and visceral co-contractions.
Trigger points can often be palpated along the anterior inferior costochondral margin.
These trigger points should be contextualized with other relationships such as:
-
Submandibular inferior margin (often on the opposite side to the diaphragm trigger points)
-
Abdominal visceral fascia (greater and lesser omenta)
-
Spinal muscles (especially mid lumbar)
-
Abdominal muscles (especially transversus and rectus abdominus)
-
Pelvic floor muscles (pelvic diaphragm)
-
Thoracic spine and rib mobility
-
Intercostal muscles
-
Serratus musculature
-
1st rib mechanics
-
Scalenes, levator scapulae, and upper trapezius

Breathing patterns are often abnormal. Hyperventilation syndrome, panic attacks, and postural habit are increasingly diagnosed.
If untreated, these syndromes also have ongoing physiological consequences, such as respiratory alkalosis (too much carbon dioxide is exhaled by over-breathing).
Paradoxically, this situation is one of the key factors in the development of chronic myofascial trigger points throughout the body.
It may be interesting to note here that cranial osteopaths talk about eight diaphragms which all coordinate together in breathing: the diaphragma sellae, under the pituitary gland; the submandibular myofascial raphe, bilaterally; the thoracic inlet/outlet, bilaterally; the abdominal diaphragm; and the pelvic floor, bilaterally.
Abnormal breathing and trigger point formation
Garland (1994) suggested a sequence of musculoskeletal changes that may develop over time as a result of chronic upper chest respiration:
- Restriction in thoracic spine mobility (secondary to aberrant rib mechanics)
- Trigger point formation in scalenes group, upper trapezius, and levator scapulae
- Tight and stiff cervical spine
- Changes in tone of abdominal diaphragm and transversus abdominis (Hodges et al. 2001; McGill et al. 1995)
- Imbalance between weakened abdominal muscles and hypertonic erector spinae
- Pelvic floor weakness
This trigger point therapy blog is intended to be used for information purposes only and is not intended to be used for medical diagnosis or treatment or to substitute for a medical diagnosis and/or treatment rendered or prescribed by a physician or competent healthcare professional. This information is designed as educational material, but should not be taken as a recommendation for treatment of any particular person or patient. Always consult your physician if you think you need treatment or if you feel unwell.
Find a Trigger Point Professional in your area
Dry Needling for Trigger Points
Certify as a Trigger Point Therapist
About Niel Asher Education
Niel Asher Education (NAT Global Campus) is a globally recognised provider of high-quality professional learning for hands-on health and movement practitioners. Through an extensive catalogue of expert-led online courses, NAT delivers continuing education for massage therapists, supporting both newly qualified and highly experienced professionals with practical, clinically relevant training designed for real-world practice.
Beyond massage therapy, Niel Asher Education offers comprehensive continuing education for physical therapists, continuing education for athletic trainers, continuing education for chiropractors, and continuing education for rehabilitation professionals working across a wide range of clinical, sports, and wellness environments. Courses span manual therapy, movement, rehabilitation, pain management, integrative therapies, and practitioner self-care, with content presented by respected educators and clinicians from around the world.
Known for its high production values and practitioner-focused approach, Niel Asher Education emphasises clarity, practical application, and professional integrity. Its online learning model allows practitioners to study at their own pace while earning recognised certificates and maintaining ongoing professional development requirements, making continuing education accessible regardless of location or schedule.
Through partnerships with leading educational platforms and organisations worldwide, Niel Asher Education continues to expand access to trusted, high-quality continuing education for massage therapists, continuing education for physical therapists, continuing education for athletic trainers, continuing education for chiropractors, and continuing education for rehabilitation professionals, supporting lifelong learning and professional excellence across the global therapy community.

Continuing Professional Education
Looking for Massage Therapy CEUs, PT and ATC continuing education, chiropractic CE, or advanced manual therapy training? Explore our evidence-based online courses designed for hands-on professionals.