Trigger Point Therapy - Subacromial Impingement
Shoulder Impingement Explained - Dr. Jonathan Kuttner MD
Subacromial impingement syndrome is the most common shoulder complaint in orthopedic clinics (44–65%) and the most frequent cause of shoulder pain in over-arm athletes
Subacromial impingement problems are particularly common, most especially with those who participate in throwing or racket sports, but also as a result of work related trauma and overuse.
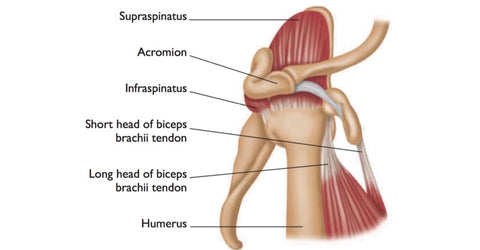
Compression of the narrow subacromial space on the top of the shoulder between the head of the humerus and the acromion of the scapula results in local pain and loss of coordination in the rotator cuff muscles of the shoulder.
Tissue trauma associated with it includes damage to the glenoid labrum, the tendon of the long head of biceps brachii and the subacromial bursa.
Dysfunction and damage in the muscles of the rotator cuff can cause the humeral head to displace upward during elevation of the arm, leading to irritation of structures in the subacromial space such as the supraspinatus tendon and subacromial bursa.
Cause of injury
Repeated overhead movements as in tennis, swimming, golf, weightlifting and house-painting. Irritation of the rotator cuff due to throwing sports including baseball. Underlying predisposition, including rheumatoid arthritis.
Signs and symptoms
Shoulder pain and difficulty raising the arm in the air. Pain during sleep when the injured arm is rolled on. Pain during rotational movements such as reaching into a back pocket.
Complications if left unattended
Increasing stiffness of the joint and further loss of motion may result should impingement be ignored. Rotator cuff tendons may be torn should athletic activity be undertaken prior to full recovery.
Tendinitis and bursitis frequently develop with impingement as a pre-condition. This may be related to trigger point formation (see below).
Rehabilitation and prevention
Following a period of healing, various forms of manual therapy and trigger point therapy may be used to help restore strength and range of motion in the affected rotator cuff, and to accelerate healing.
Avoiding or limiting repetitive motions that cause rotator cuff irritation may help prevent the injury. Strengthening exercises and light-weight training to strengthen the muscles of the rotator cuff are also useful preventive measures.
Long-term prognosis
Typically, the condition shows marked improvement within 6–12 weeks. However, trigger points will often form on the rotator cuff muscles as part of the body's self-protection mechanism.
Where left untreated, these trigger points may actually cause the condition to reoccur or lead to other shoulder complications.
Trigger Points
Impingement often results in the formation of trigger points in the rotator cuff muscles, which remain for some time even after the impingement has cleared.
Trigger points can occur quite quickly, with causes ranging from the ball of the joint being pressed on to the cuff tendon through sleeping awkwardly, to a tweak to the tendon during an overhead shot in badminton.
Actions such as these can cause a small amount of swelling and pain, which can cause temporary muscle inhibition in order to protect the shoulder, increasing the risk of further injury from a change in the abduction cycle.
Trigger points will commonly develop in the broad flat bellies of the supraspinatus and infraspinatus muscles, and the middle fibers of the thick trapezius muscle.
Find a Trigger Point Professional in your area
Dry Needling for Trigger Points
Certify as a Trigger Point Therapist
NAT Online Trigger Point Courses:
This trigger point therapy blog is intended to be used for information purposes only and is not intended to be used for medical diagnosis or treatment or to substitute for a medical diagnosis and/or treatment rendered or prescribed by a physician or competent healthcare professional. This information is designed as educational material, but should not be taken as a recommendation for treatment of any particular person or patient. Always consult your physician if you think you need treatment or if you feel unwell.
About Niel Asher Education
Niel Asher Education (NAT Global Campus) is a globally recognised provider of high-quality professional learning for hands-on health and movement practitioners. Through an extensive catalogue of expert-led online courses, NAT delivers continuing education for massage therapists, supporting both newly qualified and highly experienced professionals with practical, clinically relevant training designed for real-world practice.
Beyond massage therapy, Niel Asher Education offers comprehensive continuing education for physical therapists, continuing education for athletic trainers, continuing education for chiropractors, and continuing education for rehabilitation professionals working across a wide range of clinical, sports, and wellness environments. Courses span manual therapy, movement, rehabilitation, pain management, integrative therapies, and practitioner self-care, with content presented by respected educators and clinicians from around the world.
Known for its high production values and practitioner-focused approach, Niel Asher Education emphasises clarity, practical application, and professional integrity. Its online learning model allows practitioners to study at their own pace while earning recognised certificates and maintaining ongoing professional development requirements, making continuing education accessible regardless of location or schedule.
Through partnerships with leading educational platforms and organisations worldwide, Niel Asher Education continues to expand access to trusted, high-quality continuing education for massage therapists, continuing education for physical therapists, continuing education for athletic trainers, continuing education for chiropractors, and continuing education for rehabilitation professionals, supporting lifelong learning and professional excellence across the global therapy community.

Continuing Professional Education
Looking for Massage Therapy CEUs, PT and ATC continuing education, chiropractic CE, or advanced manual therapy training? Explore our evidence-based online courses designed for hands-on professionals.